Hip Replacement is one of the most successful Surgeries in orthopedics. In this Surgery, the surgeon removes the damaged part of the hip and replaces it with an artificial hip. This relieves pain and improves the movements of the hip joint.
When should you get a hip replacement?
1. When the pain in your hip and groin interferes with daily activities, such as walking, sitting, and resting.
2. When you have stiffness in your hip, which restricts your mobility.
Our Normal Hip Anatomy
Our hip joint is a ball-and-socket joint. On top is the socket, the acetabulum (part of the pelvis bone). Inside this socket moves a ball known as the femur head (part of the femur—thigh bone). The hip movement is due to the ball’s movement inside the socket.
In a normal hip, the surfaces of the socket and the ball are covered with a tissue known as cartilage. The cartilage layer is responsible for painless and smooth joint movements. Damage or wear and tear of the cartilage leads to arthritis, which causes pain and restriction of joint movement.
In what conditions hip replacement is done?
1. Osteoarthritis—It occurs due to age-related wear and tear of the hip joint. It usually occurs in the older population and in people with a history of arthritis. The cartilage covering the joint surface gets damaged and eroded, leading to pain in the joint.
2. Osteonecrosis (AVN) – The blood supply to the femur head can be reduced due to various causes such as fracture, dislocation, excessive drinking, and excessive steroid use. This lack of blood weakens the bone and leads to the collapse of the femur head. The irregular surface of the femur head rubs on the acetabulum and causes joint destruction.
3. Rheumatoid arthritis is an autoimmune disease in which the synovial membrane gets inflamed and starts damaging the joint cartilage. In long-standing and untreated diseases, the cartilage damage gets extensive, causing pain and complex hip movements.
4. Post-trauma—Fractures of the neck of the femur in particular age groups are treated with hip replacement. Hip arthritis after an acetabulum fracture may require hip replacement in some people.
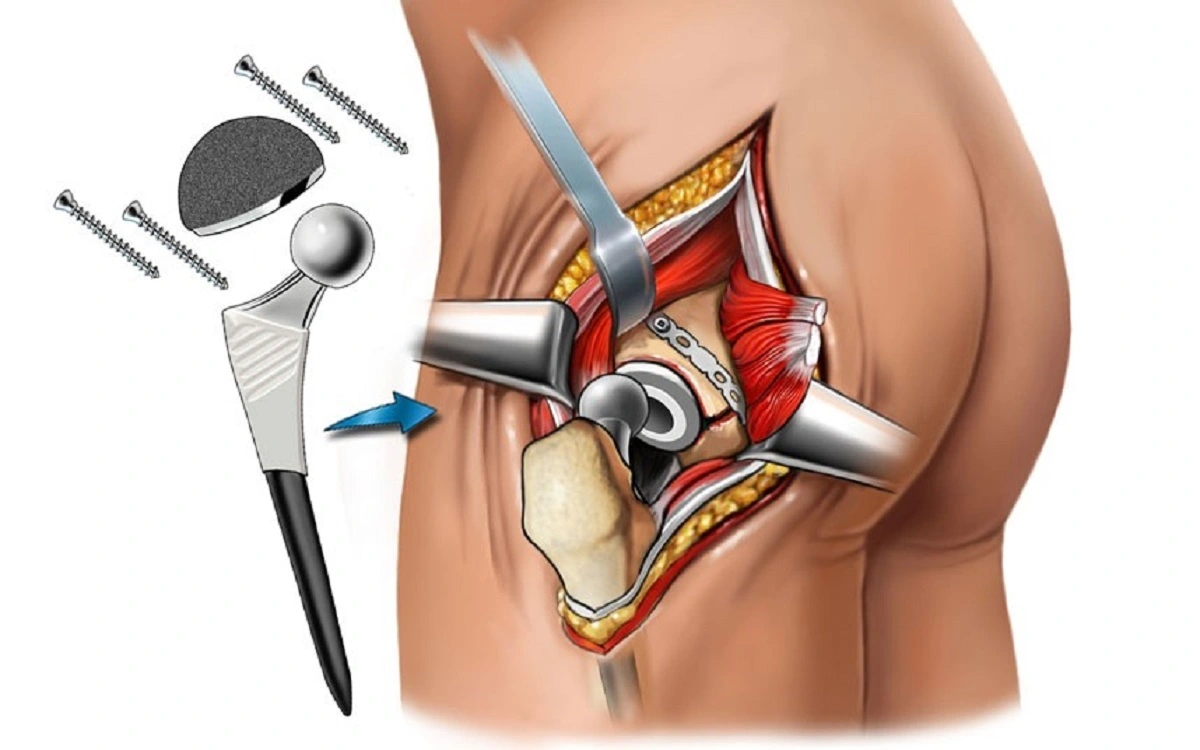
What are the components of hip replacement?
· The damaged femoral head is removed and replaced with a metal or ceramic head. This new head is fixed with a metal stem in the femur (thigh bone). The metal stem can either be fixed using cement (Cemented hip replacement) or press-fit into the bone (Un-cemented Hip replacement).
· The damaged cartilage surface of the acetabulum is removed and replaced with a metal socket. This socket is fixed using cement and screws, or it can be press-fit into the bone.
· A spacer is inserted between the femur head and the acetabulum, which is responsible for smooth hip motion. This spacer can be made of ceramic or very high-quality plastic.
In Total Hip Replacement,, the femur head and the acetabulum surface are replaced,, but in Hemiarthroplasty,, only the femur head is replaced.
What is the evaluation before Surgery?
· History – Your surgeon will take a detailed history regarding your condition. He will ask questions about your pain and the problems you face in your daily activities.
· Physical examination: Your hip will be examined for tenderness, strength, and range of motion.
· Imaging—Radiographs will be taken of your joint to assess joint damage. Advanced imaging, such as CT or MRI, may be needed in some patients.
· Blood tests—When planning Surgery, additional tests such as blood tests, ECG, and Chest X-rays will be done to check your fitness for the Surgery. In older populations, advanced tests such as 2D-ECHO may also be required. If you have any co-morbidities, such as diabetes, hypertension, etc., they need to be controlled before the Surgery.
Realistic Expectations After Surgery
Most patients who undergo hip replacement experience a dramatic reduction in pain and improvement in their ability to perform their daily activities. Patients can walk, drive, bike, swim, play golf, and do other low-impact activities.
An artificial joint is prone to wear and tear like a typical joint. High-impact activities increase this process and, in turn, decrease the life of the implant. Therefore, patients are advised against high-impact activities such as jogging, running, jumping, etc.